Tuberous sclerosis also
known as Bourneville disease is a rare phacomatosis characterized by
development of benign tumours1 affecting multiple organ systems
including skin, brain, retina, kidney, heart and lungs. It may present in
sporadic (60%) or autosomal dominant (40%) manner with a prevalence of 1 in
60001 live births affecting both sexes and all ethnicities. We
report a case of an 11-year-old boy with distinctive clinical and radiological
features of tuberous sclerosis.
CASE REPORT
An 11-year-old boy presented to our OPD
with complaints of blurring of vision in both eyes for past few months and
headache and vomiting for 15 days. Headache and vomiting were more noticeable
in early morning after waking from sleep. He also had abdominal pain for 15
days.
On general physical
examination, multiple well-defined brownish papules were seen on nose and
cheeks in a typical butterfly pattern. A fibrous patch of around 2cm was
present on forehead and right cheek. A skin tag was present in left
preauricular area. A nodular growth involving nail bed of left fourth digit was
seen. On ocular examination his best-corrected visual acuity was 6/18 OD with
-1.00 DS/-0.50 DC x30 and 6/9 OS with -1.00 DS. Anterior segment of both eyes
was normal. On dilated fundus examination, established papilledema was seen. He
was advised to get an MRI Brain done. MRI Brain revealed non-communicating
hydrocephalus secondary to intraventricular mass most likely a sub-ependymal
giant cell astrocytoma. It also showed multiple sub-ependymal nodules. For
abdominal pain, he was referred to pediatrician who advised him abdominal ultrasound
followed by a CT scan abdomen, which revealed the presence of a large extra-renal
hamartoma. Parents also gave history of seizures since childhood for which the
child had taken sodium valproate for some time. Currently, EEG revealed non-focal
seizure pattern. Heart and lung imaging was normal. The child was result of a
non-consanguineous marriage and no family member had similar manifestations. On
the basis of above findings diagnosis of tuberous sclerosis was made. For the
hydrocephalus, ventriculo-peritoneal shunt surgery was planned by neurosurgery
department. For the extra-renal hamartoma, observation with yearly CT Abdomen
was advised by the pediatric oncologist. For early detection of retinal
hamartomas, yearly fundoscopy was advised.
Table 1: Diagnostic criteria for tuberous
sclerosis1.
|
Major Features |
Minor Features |
|
Hypo-melanotic macules (>3 at least
5mm diameter) |
Confetti skin lesions |
|
Angiofibromas (>3) or fibrous
cephalic plaque |
Dental enamel pits (>3) |
|
Ungual fibromas > 2 |
Intraoral fibromas (>2) |
|
Shagreen patch |
Retinal achromic patch |
|
Multiple retinal hamartomas |
Multiple renal cysts |
|
Cortical dysplasias |
Non-renal hamartomas |
|
Sub-ependymal nodules |
|
|
Sub-ependymal giant cell astrocytoma |
|
|
Cardiac rhabdomyoma |
|
|
Lymphangioleiomyomatosis (LAM) |
|
|
Angiomyolipomas>2 |
|
DISCUSSION
TSC is characterized by hamartomas of
multiple organs from all primary germ layers2. It is an autosomal
dominant disorder with nearly complete penetrance with variable expressivity. The
mutation3,10 in genes TSC1 encoding hamartin and TSC2 encoding
tuberin result in formation of hamartomas in various organs. The classic triad4,8
of epilepsy, mental retardation and adenoma sebaceum is seen in only a minority
of patients.
TSC has dermatological
manifestations1,6 like hypomelanotic macules (Ash leaf spots; 90%),
facial angifibromas (adenoma sebaceum; 75%), ungula hamartomas (20%), skin
tags, Shagreen patch (50%)

Fig. 1: Clinical photograph
of the patient showing adenoma sebaceum, right cheek fibrous plaque, left
preauricular skin tag and ungual fibroma.
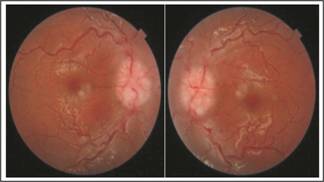
Fig. 2: Fundus photographs showing
papilledema.
and cafι-au-lait
macules. Hypo-melanotic macules are at least 5mm in size and typically appear
at birth or in infancy on limbs, trunk or scalp. Adenoma sebaceum appear
between two and five years as fibro-angiomatous red papules in a butter fly
distribution around nose and cheeks. Shagreen patch is an area of diffuse
thickening over lumbar region having an orange peel appearance that usually
appears in first decade of life. Fibrous cephalic plaques can be seen on
forehead as well as face in about 25%. Subungual and
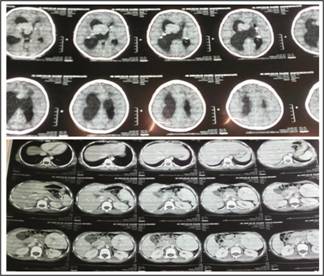
Fig. 3: CT Brain showing subependymal nodules and giant cell astrocytoma.
CT Abdomen showing nonrenal abdominal hamartoma.
periungual fibromas1 appear in
second decade or later. Confetti skin lesions are hypo-pigmented macules of 1
to 3 mm in size5. In oral cavity, dental enamel pits and fibromas
may be seen. Among ocular findings1, retinal astrocytoma, retinal
achromic patch, patchy iris hypopigmentation and atypical iris coloboma may be
seen. Sub-ependymal nodules1 (SEN; 80%) are benign growths that may
be detected prenatally or at birth. Sub-ependymal giant cell astrocytomas1
(SEGA; 5-15%) arise from SEN mostly during childhood or adolescence. They are
benign and slow growing but can cause obstructive hydrocephalus. Seizures,
learning difficulties, mental retardation and psychiatric disturbances can be
present8,9. Cardiac rhabdomyomas1 are frequently seen
during prenatal life but regress later on and may cause arrhythmias. Pulmonary lymphangioleio-myomatosis1
may be seen. Angiomyolipomas1 usually affect kidneys but can affect
other organs too. Multiple renal cortical cysts can be present too.
Updated diagnostic criteria1
according to the recommendations of 2012 International TSC Consensus Conference
is given in table 1. Two major or one major with two minor features make a
definite diagnosis.
Our patient had three major features
including facial angiofibromas/fibrous cephalic plaque, subependymal nodules,
subependymal giant cell astrocytoma and one minor feature i.e., non-renal
abdominal hamartoma which led us to the clinical diagnosis of definite TSC.
Ungual fibroma and renal cortical cyst were also present but they did not meet
the criterion.
It is quite evident from
our case report that an array of findings can be seen in tuberous sclerosis.
The approach to management is therefore multidisciplinary and symptomatic to a
large extent. Likewise, the quality of life depends on the particular
manifestations in a patient.
Authors Affiliation
Dr. Rabia Chaudhry
Consultant Ophthalmologist
Jinnah
Postgraduate Medical Centre, Karachi.
Dr. Areej Riaz
Postgraduate resident
Jinnah Postgraduate Medical Centre,
Karachi.
Role of Authors
Dr. Rabia Chaudhry
Diagnosis
and management
Dr. Areej Riaz
Data collection and manuscript writing
REFERENCES
1.
Northrup H, Krueger DA. Tuberous Sclerosis Complex Diagnostic Criteria Update:
Recommendations of the 2012 International Tuberous Sclerosis Complex Consensus
Conference. Pediatr Neurol. 2013 Oct; 49 (4): 243-54.
2.
Leung AKC, Robson LM.
Tuberous Sclerosis Complex: A Review. J Pediatr Health Care, 2007; 21: 108-114.
3.
Illahi Y, Tanveer S, Khurshid PKA, Naeem A, Ali N. Tuberous sclerosis. Classical presentation in a male patient. NMJ.
2010; 2: 29-32.
4.
Jankar AN, Palange PB, Purandare VC. Tuberous sclerosis- A case report. Int J Biomed Res. 2014; 5: 649-50.
5.
Cheng TS.
Tuberous sclerosis complex: An update. Hong Kong J Dermatol Venereol. 2012; 20:
61-7.
6.
Sarkar S, Khaitan T, Sinha R, Kabiraj A. Tuberous sclerosis complex: A case report. Contemp Clin Dent.
2016 Apr-Jun; 7 (2): 236-34.
7.
Syed KN.
Tuberous sclerosis. J Pak Med Assoc. 2010 Aug; 60 (8): 683-85.
8.
Zeebaish S, Hemalatha P, Anusha Y, Surendra RN, Durga Prasad TS. Case report on tuberous sclerosis. Int J Basic Clin Pharmacol.
2017 Apr; 6 (4): 997-1000.
9.
Roach E, Sparagana S.
Diagnosis of tuberous sclerosis complex. J Child Neurol. 2004; 19: 643-9.
10.
Li C, Liao S, Yu J.
Tuberous sclerosis complex confirmed by genetic analysis: a case report. J Neurol Neurosci. 2016; 6: 4.